This week’s practice question covers the topic of cost effectiveness in healthcare. Why cover cost effectiveness?
Well first, cost effectiveness fits into clinical informatics as a form of clinical decision support. More specifically, it falls under the category of “decision science” in the clinical informatics core content and is therefore on the exam—-so you should know it. Secondly, it can be handy when evaluating possible decisions regarding patients or the organization.
Let’s first discuss some background on what cost effectiveness is (without giving away any answers, of course).
Cost effectiveness is an economic analysis that compares effects (relative costs and outcomes) to courses of action. It allows us to estimate the costs and outcomes of interventions.
Rather than assign a dollar value to the relative costs and outcomes, cost effectiveness analysis typically uses Quality Adjusted Life Years (QALYs) as an alternative. This avoids inappropriately placing a dollar value on someone’s health or life.
A cost effectiveness analysis expresses its result in a ratio:
(cost associated w/health gain)
(outcome or gain in health from a measure)
It can also be used to measure the incremental costs and outcomes associated with particular interventions.
(cost associated w/health gain scenario B – cost associated w/health gain scenario A)
(outcome or gain in health from scenario B – outcome or gain in health from scenario A)
In both formulas, outcomes must be considered separately. They cannot be combined.
The lower the ratio, the better. For example, a ratio where each QALY costs $20,000 is better than a ratio where each QALY costs $200,000.
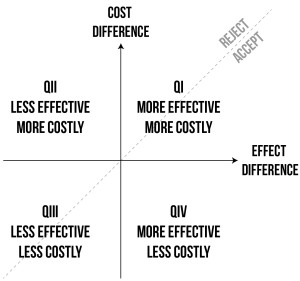
Results of a cost effectiveness analysis are sometimes charted into a four-quadrant graph. We’ll cover this a little bit more in the explanation. For now, I think we may have even given you too much information to solve this week’s questions, but let’s get into it anyway.
Question
A healthcare group is considering adding some additional guidelines into their clinical decision support system. One guideline includes testing children for hypercholesterolemia which is expected to gain one QALY at a cost of $35,000. The second testing guideline includes testing children with risk factors for obesity for type II diabetes. This is expected to gain 10 QALYs at a cost of $275,000. The third guideline implements a weight management program with regular exercise programs that is expected to gain 20 QALYs at a cost of $650,000. Which of the guidelines should be implemented based on cost effectiveness alone?
A. Hypercholesterolemia Testing
B. Diabetes Type II Testing
C. Weight Management Program Implementation
D. None of these would be cost effective
Answer and Explanation
Remember, cost effectiveness = Cost associated/outcome or gain in health
A. $35,000/1 = 35,000
B. $275,000/10 = 27,500
C. $650,000/20 = 32,500
D. All guidelines can be analyzed for cost effectiveness, so this would not be a valid answer.
Therefore, the answer to this question is B – Diabetes Type II testing. It has the potential to save the greatest number of quality years of life for patients in proportion to the cost.
If you’re comparing many different options, it may be helpful to use a chart to analyze your findings. A chart like the one below helps display which options should be accepted and which should be rejected.
If you’re looking for other study resources, check out some of our other practice questions of the week. You can also purchase our text – Clinical Informatics Board Review: Pass the Exam the First Time. It’s the only board review book for the clinical informatics exam. It also comes with a money back guarantee if you don’t pass the exam on your first attempt – the only study material for the clinical informatics exam with one. You can also sign up for practice questions through learn.informaticspro.com if you’re looking to test your readiness for the exam.
Resources
If you’re looking for more information on cost-effectiveness analysis, check out these links.
CDC. “Part V: Effectiveness Analysis Slides.
Moalek, Mo. Evidence Based Medicine UK. Implementing QALYs