While the clinical informatics subspecialty is a newcomer to the medical specialty arena, it’s introduction has been a long time in the making.
The recording of healthcare data has been around since Hippocrates first developed the medical record in the fifth century. Since then, records have evolved from tablets and paper ledgers to the Electronic Health Records (EHRs) we’re so used to seeing in today’s health care environment.
However, clinical informatics has a lot more history behind it than you may realize. In this post, we’ll cover some of the highlights without getting too in-depth.
While clinical informatics is by no means only about EHRs and the data we can mine from them, it is often the first thing that often pops into our head regarding the subject. Plus, it makes a good base from which we can build. So let’s get started.
A (Very Brief) History of EHRs
As computing power increased in the mid to late-1900s, GUIs (Graphical User Interfaces) became more prominent and individuals and organizations began to see the opportunities associated with large amounts of health information in digital form. EHRs began to take off. Dr. Clem McDonald from the Regenstrief Institute summed up nicely the goals and benefits of EHRs:
“Our goal was to solve three problems: (1) to eliminate the logistical problems of the paper records by making clinical data immediately available to authorized users wherever they are – no more unavailable or undecipherable clinical records; (2) to reduce the work of clinical book keeping required to manage patients – no more missed diagnoses when laboratory evidence shouts its existence, no more forgetting about required preventive care; (3) to make the informational ‘gold’ in the medical record accessible to clinical, epidemiological, outcomes and management research.”
These benefits could be huge to the health care field. But that’s not to say they were without their challenges…
Innovators such as Lockheed, 3M, Regenstrief, and the VA began developing systems to capture and organize digital health information. As the business case for EHRs became clear, more and more commercial companies began developing their own EHRs to sell to hospitals and other health care organizations.
This commercialization period presented multiple challenges – many of which are still very apparent today. For one, there was very little transparency into these systems. This resulted in a lack of standards in EHRs as no vendor would give away their software’s “secret sauce”. Interoperability between vendors was very difficult, if not impossible. Configurations, units of measurement, and styles of recording between vendors and even within and between health care systems have made the conversion from written record to electronic health record one of the greatest challenges in the health information technology industry.
In addition to this lack of standards, EHRs presented another challenge: each user of EHRs had their own workflow, therefore, “plug-and-play” systems were ineffective, as each system or user would need a customized solution.
Wouldn’t it be great if we could go back in time and base all of our systems off of standards!
Unfortunately we can’t, but clinical informatics is working on the standards part.
The Introduction of Clinical Decision Support
In the 80’s EHRs evolved from vehicles from which to store health information to repositories from which advanced expert systems could pull from to provide clinical decision support and assistance to health care providers.
The first research on diagnostic decision-making – “Reasoning Foundations of Medical Diagnosis,” reviewed methods that could be used where risk and uncertainty existed. This paper began the conversation on computer-based clinical decision support.
Following this, additional papers were published in the mid-80’s that included topics in medical informatics frameworks, functional and architectural considerations for clinical information systems, medical research analysis, and standardizing electrocardiogram analyses from computers.
Now, Clinical Decision Support Systems are often integrated directly with EHRs. Alerts, reminders, and pop-ups created from CDS can improve the care that patients receive if implemented well. If not, they may remind a provider of a bad geocities webpage from the early ’90s.
Practitioners of clinical informatics seek to take these alerts and reminders and seamlessly integrated them into clinical workflows so providers can do their jobs safely while the technology runs virtually invisibly in the background.
The Birth of Professional Informatics Associations
The first health informatics organizations were born in the early 1950s. The first of which was founded in Germany during 1949 by Dr. Gustav Wagner. More and more beginning to appear during the 1960s and 70s across Europe and the United States. The largest and most prominent professional organization from this time is the International Medical Informatics Association (IMIA).
In 1989, the American Medical Informatics Association (AMIA) was formed as the United States representative to IMIA through the integration and merging of the following informatics organizations:
- American Association for Medical Systems and Informatics
- American College of Medical Informatics
- Symposium on Computer Applications and Medical Care
The Evolution of Clinical Informatics as a Subspecialty
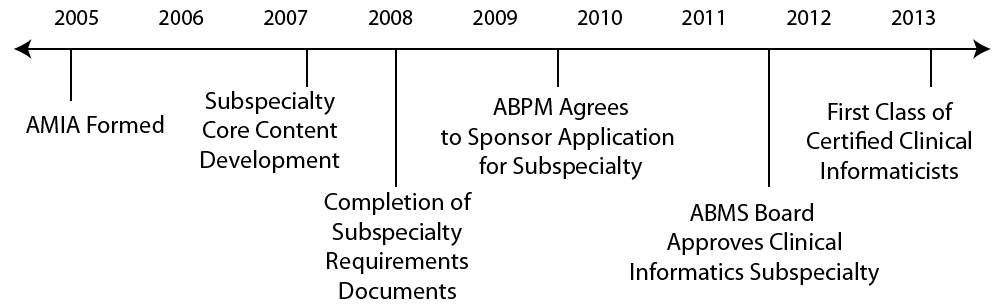
In 2005, AMIA began the process to make clinical informatics a recognized subspecialty of the American Board of Preventative Medicine by the American Board of Medical Specialties. In 2013, the process was complete and the first diplomates in the subspecialty in clinical informatics received their certification.
In 2014, the second class of delegates (306 of them to be exact) became board certified in clinical informatics.
Where Will the Future of Informatics Be?
New technologies and new regulations have created new opportunities in informatics for anyone looking to change the future of health care.
- Machine learning and natural language processing is helping us wrap our mind around impossibly large sets of data and extract usable pieces of knowledge. Startups like lumiata, clinigence, AgileMD and Zipnosis are working to improve the ways we do this through better access to and analysis of healthcare data. Whether these will eventually replace tasks of health care providers (or even their jobs) is the big question. Don’t believe it? Check out this article from the economist. It will get you thinking.
- HITECH, Meaningful Use, the HIPAA privacy and security rules, and the Affordable Care Act have rapidly accelerated the adoption of health IT.
- The clinical informatics subspecialty teaches physicians to lead organizations through massive IT and organizational change, mine data from EHRs and other clinical information systems to find previously undiscovered correlations, or develop systems to improve the accessibility and affordability of health care to patients around the globe.
Where the future of informatics heads is up to people like you who are looking to change the future of health care using technology. The question is: where will you take us?
References:
Garner, R.M., Overhage, J.M., Steen, E.B., Munger, B.S., Holmes, J.H., Williamson, J.J., Detmer, D.E. (2009). Core content for the subspecialty of clinical informatics. Journal of the American Medical Informatics Association. Vol 16 No 2. DOI 10.1197
National Institutes of Health National Center for Research Resources (2006). Electronic health records overview. www.himss.org
Ledley, R.S. and Lusted, L.B. Reasoning Foundations of Medical Diagnosis. Science. 130 (1959) 9021.
Haux, R. Medical informatics: past, present, future. International journal of Medical Informatics. 79 (2010) 599-610.
Tripathi, Micky. “EHR Evolution: Policy and Legislation Forces Changing the EHR.” Journal of AHIMA 83, no.10 (October 2012): 24-29.